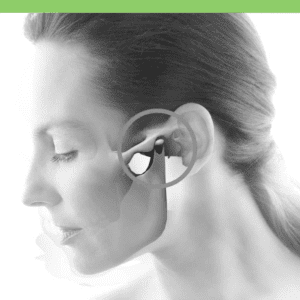
 TMJ stands for the two temporomandibular joints, one on each side of the jaw. These joints act like a sliding hinge, connecting your lower jawbone (mandible) to the temporal bone in front of your ears. If you place your fingers just in front of your ears and open your mouth, you can feel the joints. When there are problems in these joints, it is called a temporomandibular disorder or TMD.
TMJ stands for the two temporomandibular joints, one on each side of the jaw. These joints act like a sliding hinge, connecting your lower jawbone (mandible) to the temporal bone in front of your ears. If you place your fingers just in front of your ears and open your mouth, you can feel the joints. When there are problems in these joints, it is called a temporomandibular disorder or TMD.
Because these joints are flexible, the jaw can move smoothly up and down and side to side, enabling us to talk, chew and yawn. Muscles attached to and surrounding the jaw joint control its position and movement. The rounded ends of the lower jaw are called condyles. There is a soft disc between the condyle and the temporal bone that acts as a shock absorber from chewing and other movements.
The temporomandibular joint is different from the body’s other joints. The combination of hinge and sliding motions makes this joint among the most complicated in the body. Also, the tissues that make up the temporomandibular joint differ from other load-bearing joints, like the knee or hip. Because of its complex movement and unique makeup, the jaw joint and its controlling muscles can pose a tremendous challenge to both patients and health care providers when problems arise.
It is estimated that more than ten million Americans may be affected. Women are more affected by TMJ than men. Patients may have one or more of the disorders of the TMJ that fall into three main categories:
- Pain or discomfort in the muscles that control jaw function
- Joint damage: Displaced disc, bone dislocation, and/or injury to condyle
- Disease: Arthritis damage to cartilage or connective tissue disorders
SYMPTOMS:
Exact causes are not known, but dentists believe symptoms come from problems with the muscles in the jaw or with the joint and/or its parts. Injury is an obvious cause, but stress, leading to grinding or clenching teeth (which puts pressure on the joint) is also a major suspect. Some of the symptoms include:
- Pain or tenderness in your face, jaw joint area, neck and shoulders
- Pain in or around the ear when you chew, speak, or open your mouth wide
- Swelling on the side of your face
- Not being able to open your mouth wide
- Jaws that get “stuck” or “lock” in the open- or closed-mouth position *
- Clicking, popping, or grating sounds in the jaw joint when you open or close your mouth or chew (may or may not be painful). **
- A tired feeling in your face
- Jaw muscle stiffness
- A change in the way the upper and lower teeth fit together
- Toothaches, headaches, neck aches, dizziness, earaches, hearing problems, tinnitus
* Not to be confused with Lockjaw (the bacterial disease, Tetanus – contracted through a cut or wound, affecting the nervous system). The infection causes severe muscle spasms, leading to “locking” of the jaw, making it hard to open the mouth or swallow. In severe cases, tetanus infections may lead to death by suffocation. Immediate medical attention is imperative. Prevented by the vaccine DTaP.
** Jaw noises alone, without pain or limited jaw movement, do not indicate a TMJ disorder and do not warrant treatment.
DIAGNOSIS:
If you are diagnosed with a TMJ disorder, a CT scan can provide detailed images of the bones involved in the joint, and MRIs can reveal problems with the joint’s disk. Your dentist or doctor will also do a clinical exam that may include:
- Listening for sounds in your jaw when you open and close your mouth
- Observing the range of motion in your jaw
- Pressing on areas around your jaw to identify sites of pain or discomfort
- TMJ arthroscopy *
* During TMJ arthroscopy, a small thin tube (cannula) is inserted into the joint space, and a small camera (arthroscope) is then inserted to view the area and diagnose the problem.
Consult with your doctor to rule out other known causes of pain. Facial pain can be a symptom of many conditions, such as sinus or ear infections, various types of headaches, and facial neuralgias (nerve-related facial pain). Ruling out these problems first helps in identifying TMJ disorders.
TREATMENT:
In some cases, the symptoms may go away without treatment, but if they persist, your doctor may recommend a variety of treatment options, often doing more than one at the same time, usually starting with nonsurgical options such as medications:
Pain and anti-inflammatories, OTC or prescription
- Tricyclic antidepressants, sometimes used for pain relief
- Muscle relaxants
Non-drug therapies may include:
- Oral splints or bite guards to prevent damage from clenching and grinding *
- Physical therapy using moist heat and ice, ultrasound, exercises, etc.
- Counseling to understand and correct behaviors (like clenching and grinding) that may aggravate your pain
- Chiropractic cranial adjustment
* If a stabilization splint causes or increases pain, or affects your bite, stop using it and see your health-care provider.
Self-care practices can be helpful in easing symptoms, such as:
- Eating soft foods
- Applying ice packs
- Avoiding extreme jaw movements (such as wide yawning, loud singing, and gum chewing)
- Learning techniques for relaxing and reducing stress
- Practicing gentle jaw stretching and relaxing exercises that may help increase jaw movement
Complementary and alternative medicine techniques may help manage the chronic pain often associated with TMJ disorders, for example:
- Acupuncture
- Relaxation techniques
- Biofeedback
Even when TMJ disorders have become persistent, most patients still do not need aggressive types of treatment, but if relief is not obtained with any of the above treatments, more invasive therapies may be recommended:
- Arthrocentesis: Inserting small needles into the joint, using fluid to irrigate and remove debris and inflammatory byproducts.
- Injections: Corticosteroid, or infrequently, Botox.
- TMJ Arthroscopy: can be as effective as open-joint surgery.
- Modified Condylotomy: Surgery on the mandible but not in the joint. May be helpful for pain and if locking is present.
- Open-Joint Surgery: If there is a structural problem in the joint, to repair or replace the joint (a last resort).
Failure to respond to conservative treatments does not automatically mean that surgery is necessary. If surgery is recommended, be sure to have the doctor explain to you, in words you can understand, the reason for the treatment, the risks involved, and other types of treatment that may be available.
If treatment is needed, it should be based on a reasonable diagnosis, be conservative and reversible, and be customized to your special needs. Avoid treatments that can cause permanent changes in the bite or jaw. If irreversible treatments are recommended, be sure to get a reliable, independent second opinion.
Research by scientists is ongoing to understand TMJ disorders and pinpoint factors leading to chronic or persistent jaw joint and muscle pain, and to identify medications and treatments that are effective.
If you are interested in a correction of temporomandibular joints and the bite in Costa Rica, fill out the “Find a Dentist” form on this page. One of our patient advocates will reply to your needs.
